Top 4 Features Your Medical Rostering & Scheduling Software Should Have before Blaming the Schedulers
The burnout among healthcare workers is a growing concern, not just during the COVID-19 outbreak but persistently before and after. This often-overlooked issue results in longer wait times for patients seeking care. The sudden surge in patients isn’t something that can be controlled, much like the unpredictability of a pandemic. Yet, a significant contributor to this burnout stems from the inadequate management of medical rostering and scheduling, especially when dealing with unexpected events like sudden staff absences.
Healthcare professionals grapple not only with the inherent challenges of their roles but also with a system that sometimes seems unprepared to support them. It’s more than a logistical hurdle; it directly impacts patient care and the well-being of those dedicated to the healthcare system. Recognising the profound effect of scheduling inefficiencies on the health and efficiency of our healthcare providers highlights the urgent need for a systemic solution.
Are the Schedulers the Unseen Catalysts of Burnout?
At the heart of the matter is the prevalent use of manual processes in many healthcare rostering and scheduling systems. Daily schedules involve intricate coordination with HR for medical leaves or staff changes, estimating the resources needed for patient arrivals, and more. It’s not just a headache for schedulers; it’s a widespread problem affecting the entire healthcare system. A study by the American Medical Association starkly illustrates this point, showing that healthcare professionals facing work overload are three times more likely to experience burnout.
Schedulers’ Nightmare: Navigating Sudden Changes
Imagine a medical practitioner is suddenly absent, and everything goes haywire. The meticulously planned schedule turns into an unsolvable puzzle, leaving a gap in the workforce. Here’s the problem: if this gap isn’t quickly filled, it means not enough resources for the remaining on-duty medical staff. Their workload skyrockets, stress levels hit the roof, and the environment becomes a breeding ground for potential mistakes. But these aren’t just little slip-ups; they have real consequences, impacting patient care and treatment quality. Lives are on the line, emphasizing the urgent need for practical solutions in scheduling and rostering.
4 Key Features for Seamless Healthcare Operations
Some forward-thinking hospitals are leveraging medical rostering and scheduling software to revolutionise their staffing processes. The question then becomes: how can hospitals choose software with features that genuinely make a difference? Let’s explore the four must-have features:
- Intelligent Automation for Swift Adaptability: Swiftly adapting to unforeseen changes, such as sudden staff absences, is pivotal. Intelligent automation ensures real-time adjustments, facilitating uninterrupted patient care while effortlessly optimising staff allocation. This feature seamlessly integrates with internal systems, updating in real-time or batch mode, providing valuable insights into staff availability during unexpected events.
- Real-Time Visibility and Seamless Communication: Minimising scheduling delays and communication gaps is fundamental for operational efficiency. Real-time visibility features foster instant communication and updates, creating a fluid workflow that minimises disruptions. Integration with HR and other staffing systems enhances this by offering a comprehensive view of staff status, from medical leave to emergency situations, ensuring effective communication during sudden changes.
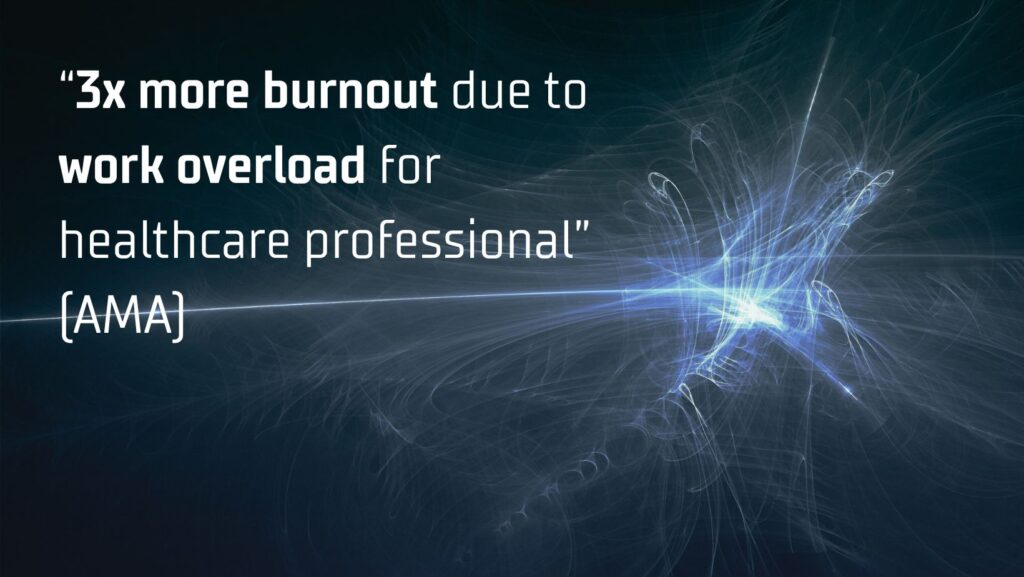
- Customisable Workflows and Agile Adaptability with Genetic Algorithm: Tailoring scheduling solutions to fit unique hospital workflows is essential. A system supporting easy updates and integration fosters agile adaptability, enabling on-the-fly adjustments to staff information in response to sudden changes. This flexibility is augmented by applying Genetic Algorithms for optimal timetables based on available resources and configurable constraints. From a study of National Library of Medicine in 2021, a hybrid genetic algorithm approach in scheduling management could outperforms the current manual scheduling in both fatigue factor and time of providing time table.
Steps of the GA algorithm – Journal of Healthcare Engineering
- Visualising Staff Distribution for Enhanced Decision-Making: Visualisation tools provide a clear insight into staff distribution through aids like bar plots, fostering informed decision-making. This feature streamlines administrative processes and enhances overall patient care quality.
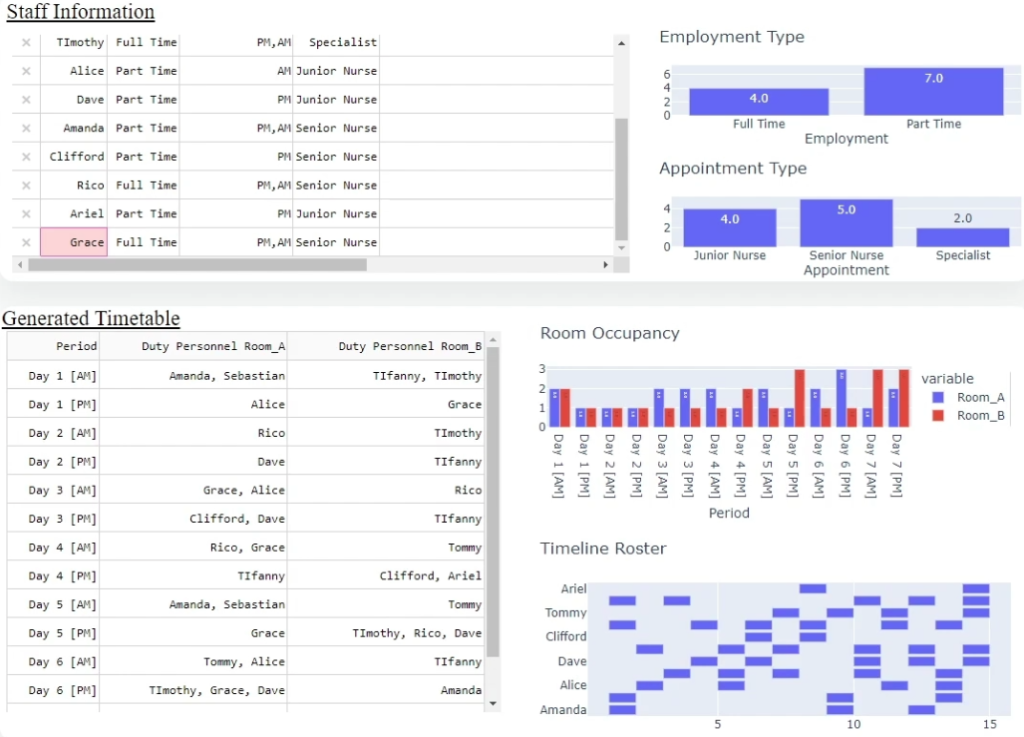
Visualisation example from KewMann AI Scheduling
Optimising Healthcare Rostering & Scheduling: Elevating Efficiency, Doubling Impact, and Ensuring Practitioners Well-Being
By embracing these features, the healthcare industry can collectively move towards a more resilient, patient-focused scheduling approach – minimising burnout, optimising resource allocation, and more patients to be cured. An Asia largest hospital has reduced more than 90% of scheduling time for healthcare schedulers, providing peace of mind while enhancing overall efficiency with KewMann. Embrace this harmonious evolution. It’s not just scheduling; it’s a prescription for a healthier, happier healthcare ecosystem.